SOAP Note: How to Write Spotless Healthcare Notes (Free Template!)
Blog: The Process Street Blog

Healthcare providers are the backbone of humanity.
It’s through their hard work, diligence, and courageousness that we’re able to recover from injuries and illnesses alike. However, even before the novel coronavirus struck, those working in the healthcare sector were run off their feet – especially considering there are only 2.6 doctors per 1,000 patients in the United States.
Healthcare providers, then, need to strike the fine balance of providing each patient with adequate care but within an appropriate timeframe.
To help make this near-impossible task a reality, many healthcare providers turn to what’s known as a SOAP note.
Not sure what a SOAP note is?
I’ve got you covered. (Spoiler: It’s not related to the cleaning product.)
In this short yet informative post, I’ll explain what a SOAP note is, its interesting history, why it’s useful, and provide a visual example of what a SOAP note looks like. To boot, I’ll also show you how Process Street makes writing and implementing SOAP notes extremely easy.
Read through the below sections to get clued-up:
- What’s the SOAP note definition?
- How a SOAP note works
- The history of the SOAP note
- The benefits of SOAP notes
- A SOAP note example
- Using Process Street for your SOAP notes (and more)!
So what’s up, Doc? Ready to get reading? 
What’s the SOAP note definition?
A SOAP (subjective, objective, assessment, plan) note is a method of documentation used specifically by healthcare providers. SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. SOAP notes, once written, are most commonly found in a patient’s chart or electronic medical records.
To see what a SOAP note template looks like, check out (and use!) this example from Process Street:
Click here to get the SOAP Note Template!
How does a SOAP note work?
To illustrate how a SOAP note works, let’s roleplay.
A patient (you) came into a medical practice with arm swelling, but no diagnosis or idea what the issue at hand could be. The physician (me) attended you and I now need to write an initial document that follows the SOAP structure.
First, I’ll be writing the subjective component. Although each component will differ depending on the patient and at which stage the note is being written (numerous notes are written at differing points until the issue is fully rectified), the subjective component often includes information such as:
- The patient’s age, race, and gender
- The CC, otherwise known as chief complaint (which, in this case, is the arm swelling)
- When the chief complaint began
- Where the chief complaint is located in the body
- The severity of the chief complaint
- Description of the chief complaint
- Relevant medical history
- And so on.
Once those basics are out the way, I can then move onto the objective component of the SOAP note. Here, I’ll be writing information on what I’ve observed from what you, the patient, are physically displaying and what you’ve verbally told me during our meeting. Plus, I’ll be writing up any findings of any examinations and tests that you’ve had done.
When writing the objective section, I’ll make to sure write down:
- Vital signs and measurements, such as blood pressure and weight
- Findings from physical examinations
- And the results from laboratory and diagnostic exams.
After that, it’s time to write notes related to assessment. Specifically, I’ll be writing:
- An analysis of the issue
- A (potential) diagnosis of the issue
- And relevant information concerning progress.
Regarding the last point, let’s, for instance, say this is your second visit to the practice regarding the issue but your first visit to me as a physician. I’ll also write a note here regarding how your state has improved or worsened since your last visit.
The fourth and final component is the plan component. It’s here that I’ll create a post-session plan. Every plan written for each patient will be entirely situational depending on who they are, what the issue is, and what stage they’re at, but plans often include:
- Medication prescriptions
- Referrals to other medical departments or personnel
- Additional/extra tests that should be conducted
- Follow-up appointments
- And whatever else is deemed necessary.
The next steps, just like the plan itself, will differ. Some medical practices may want the fully-written SOAP note to be reviewed and/or approved by a higher-up, while some practices will want the SOAP note writer to upload the completed document to a database of medical records. Or, the best plan of action may be to carry out the action tasks in the plan as soon as possible.
Either way, by following the SOAP note method of documentation, it helps to order and organize the process of note-taking that’s otherwise prone to countless human errors and mistakes!
The history of the SOAP note
The SOAP note isn’t some made-up mumbo-jumbo; rather, it has a long history rooted in the need to solve complex real-life problems faced by real-life practicing physicians on a day-to-day basis.
Here’s a short history lesson for you.
As the 1960s ended and the 70s began, Dr. Lawrence Weed stumbled upon a significant problem. As a practicing physician but also an academic researcher and teacher, he realized that not having a standardized process for medical documentation was, well, pretty sub-par.
So that physicians like him could write up notes and the information they contain quickly and in a systemized way, Dr. Weed came up with the POMR – an acronym for the problem-oriented medical record.
As Dr. Weed said himself in a Permanente Journal interview:
“The multiplicity of problems the physician must deal with every day constitutes a principal distinguishing feature between a physician’s activities and those of many other scientists. These realizations led me to develop the POMR so that medical students and practitioners could function in a structured, rigorous way more like that of workers in the scientific community.
The POMR cannot change the multiplicity of problems that physicians face. But the POMR enables a highly organized approach to that complexity.” – Dr. Lawrence Weed, Interview with Lawrence Weed, MD: The Father of the Problem-Oriented Medical Record Looks Ahead
The POMR is still used by medical organizations around the globe, and it’s what the SOAP note itself originates from.
Seeing as the SOAP note originates from the POMR, you’d be right in thinking there’s substantial overlap. However, there is variation.
To illustrate this in the simplest possible way, there are 5 main components of the POMR. These, as listed by the Imhotep Virtual Medical School, are:
- A database concerning patient history, physical tests, and laboratory exams
- A complete problem list
- Initial plans
- Daily progress notes
- And a final progress note or discharge summary.
The SOAP note, however, is different in terms of what’s required of it and the way it’s structured, despite the large overlap.
The POMR and SOAP note way of doing things also came about due to Dr. Weed’s understanding that the medical world needed to adapt to information technology. After all, if information technology can help individuals and teams complete an important process – or a collection of essential processes – more efficiently and effectively, why not harness its power?
As Dr. Weed said himself:
“I realized that medicine must transition from an era where knowledge and information processing capacity resides inside a physician’s head to a new day where information technology would provide knowledge and the processing capacity to apply it to detailed patient data.
The physicians’ unaided minds are incapable of recalling all the necessary knowledge from the literature and processing it with data from the unique patient. An epidemic of errors and waste is occurring as we persist in trying to do the impossible. Changing this requires that we recognize the crucial distinction between electronic.” – Dr. Lawrence Weed, Interview with Lawrence Weed, MD: The Father of the Problem-Oriented Medical Record Looks Ahead
With what Dr. Weed said in mind, it’s no surprise that the SOAP note picked up major traction in the 70s, as it turned the impossible into the possible (with a helping hand from IT and tech, of course).
It’s not only physicians who are using SOAP notes in the modern-day, too – it’s also behavioral healthcare practitioners to veterinarians!
The SOAP note, then, is useful for pretty much everyone in the medical field.
The benefits of SOAP notes
Now, the SOAP note wouldn’t have survived this long – nor would it be used by practitioners working in different areas – unless it’d brought about some nifty benefits.
Reader, I’m pleased to tell you my prognosis is that the SOAP note does bring multiple benefits across the board.
Specifically, these positives include:
- Orders and organizes how information is written.

- Quickens the note-taking process.

- Provides a cognitive framework for staff to follow.

- Enhances overall quality of care.

- Helps other medical professionals. 🩺
At its core, the SOAP note is all about ordering and organization. Considering tens of notes could be written by a healthcare provider on any given day, having a systemized way of writing up important notes is integral in itself. Here’s to keeping organized.
Another core element of the SOAP note is, with a structure for how to write notes, it quickens the note-taking process overall. This is because you’re not jumping to-and-fro after forgetting a certain question, and not having to go back and add to your notes after the fact because you’d forgotten to pen an important detail down.
The beauty of the SOAP note is, after following the SOAP method of documentation long enough, it starts to impact the way meetings and conversations with patients go. This means not only are your notes structured, but the way you go about interacting with patients will be, too.
By documenting all the necessary information regarding a patient and their ailment(s), you’re able to provide them with the best care possible, ensuring you’ve gotten to the heart of the problem the best you can and have created an appropriate plan of action.
SOAP notes are most often found in a patient’s electronic health record. Seeing as other medical professionals will have access to the records of the patient they’re treating, reading SOAP notes that are structured in an easy-to-read, organized way will mean they’ll know exactly what they need to do to help the patient. (Even if there’s been no other contact between the medical professionals themselves!)
Impressive list, right?
If you’re raring to learn what a SOAP note looks like in action, I’ve got you covered in the next section. 
A SOAP note example
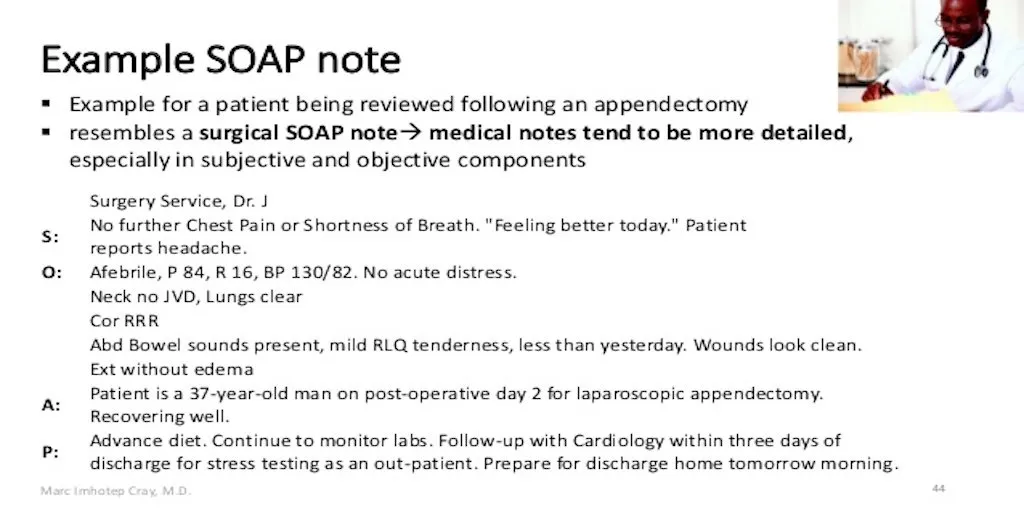
In this example, I’ll be drawing from what Marc Imhotep Cray, M.D., has written as part of his slideshow for students of the Imhotep Virtual Medical School.
Straight off the bat, you can tell that this is a surgical SOAP note, and not a medical SOAP note.
How?
Because it doesn’t contain all the details a medical SOAP would usually have, including the patient’s race, age, gender, and initial information about the chief complaint. This is because those details were most likely already written about in a previous SOAP note.
This is why the s component – that’s the subjective component, if you can’t remember – is particularly short.
The o component – objective – is rather short too, but it contains essential info on the patient’s vital signs and results from the appendectomy.
The a component – assessment – is doing exactly what it should although, again, briefly: The note writer has provided information regarding the patient’s progress and confirmed they’re doing well on their second day of recovery.
Finally, the text in the p – plan – component documents the next steps for the patient: Advancing their diet, monitoring their progress, and following up with the cardiology department before the patient is released the next day.
This example shows how SOAP notes differ depending on who’s writing them and which stage the patient is at (i.e. initial consultation versus day two of their surgery recovery). However, what binds all SOAP notes together – no matter who they’re written for, why, and at which stage – is the fact that they’re all written in a helpful, clear way.
To get started with writing proper, effective SOAP notes yourself, you’ll want to use state-of-the-art BPM software known as Process Street.
Using Process Street for your SOAP notes (and more)!
Process Street is superpowered checklists.
With Process Street, you can document workflows, business processes, and integral procedures as templates. Then, you and the rest of your team can launch an infinite number of checklists from those templates, ensuring you complete your recurring tasks to a high quality.
For a visual introduction to our nifty checklist app, watch the video below.
When it comes to writing the humble SOAP note, you can use our SOAP Note Template!
No extra material or writing lessons needed; all you need to do is sign up to Process Street for free, add the below template to your organization, and then follow its simple instructions.
Click here to get the SOAP Note Template!
Alternatively, let’s say you and your team take SOAP notes seriously.
You may want to create different SOAP note templates for the various kinds of SOAP notes there are – for instance, the aforementioned surgery SOAP note and the medical SOAP note. By doing this, you and your team can use the right template for the job and ensure the appropriate amount of detail is written!
The good news doesn’t end there, either.
What’s more is that you can use Process Street to document, follow, and complete all your important work-related processes. Every. Single. One. Be them admin-related processes such as a safety inspection or isolation area management in light of COVID-19.
To help you get started, the content team at Process Street created three medical-related template packs for you to use. These are, again, completely free and are jam-packed with Process Street’s incredible workflow automation features:
- 9 Checklists to Help Hospitals Deliver and Optimize Superb Patient Experiences
- 16 COVID-19 Procedures for Hospitals (According to Clinical Experience from FAHZU)
- 14 Client Onboarding Process Checklists for Finance, IT, Medical, SaaS, Real Estate…
If you’re unsure what I mean by “workflow automation features”, let me quickly explain.
Our templates and checklists aren’t just run-of-the-mill; they’re superpowered thanks to our in-built workflow features. These make collaborating on and completing processes even quicker and simpler.
These features include (but aren’t limited to):
- Stop tasks

- Conditional logic

- Dynamic due dates

- Task permissions

- Task assignments

- Role assignments

- Webhooks

- Embed widget

- Approvals

- And more!

To deep dive into how some of these features work, watch the following webinar.
With all the information on SOAP notes, the free Process Street templates, and your new, shiny Process Street account, you’ve got everything you and your team need to get started with writing SOAP notes.
Here’s to writing organized, clear, and spotless SOAP notes – quickly.
Do you write SOAP notes? If so, what are your thoughts on them, and do you have tips and tricks for others who are interested in implementing, writing, and using SOAP notes? Write down your comments below!